Exercise in pregnancy – risky business or risk reducing?
Historically when it comes to exercise in pregnancy women have been encouraged to stick to walking or very light exercise such as yoga or swimming. However, over the last three decades rates of pregnancy complications such as gestational Diabetes, pre-eclampsia, Gestational HT and newborn macrosomia have risen dramatically which is most likely as a result of increasing rates of maternal obesity.
Less than 15% of pregnant women meet the recommended level of weekly activity during pregnancy, and concerns such as whether exercise may increase miscarriage, growth restrictions, preterm birth, fatigue, harm to the foetus have all served as barriers to exercise in pregnancy.
In uncomplicated pregnancies, these concerns, have simply not been substantiated by the research, and in fact not participating in exercise during pregnancy may pose a bigger risk to the health of the mother and her unborn child.
The health benefits of exercise in pregnancy are huge including reduced risk of gestational diabetes, maintenance of fitness and strength, management of weight gain, reduced risk of preeclampsia, reduced rates of back pain, improved mental health and many more. Regular exercise has also been correlated to shorter and less complicated labours and fewer neonatal complications. If that’s not a reason to exercise, then I’m really not sure what is.
Taking all of these factors into account in an era of increasing BMI, and increased lifestyle diseases associated with being sedentary encouraging women to exercise in pregnancy should be an absolute health priority. I would argue that not exercising in an uncomplicated pregnancy is actually risk-reducing rather than risk increasing so it is imperative that we get the evidence-based information out there and ensure pregnant mummas are moving.
Now, there are absolutely situations when where exercise is contraindicated, this is why it is important to ensure you have discussed exercise with your medical professional to ensure you are not a “high risk” pregnancy and safe to proceed. These will include:
There are also cases that if the following symptoms occur during exercise that it needs to stop:
For the majority of women, the most recent Australian pregnancy guidelines state that all women without complications participate in regular aerobic and strength conditioning exercise during pregnancy. They also state that women should be advised that there is no evidence that regular exercise during an uncomplicated pregnancy is detrimental to the woman or foetus.
As discussed, exercise in pregnancy has many clinical benefits, however it is important that women exercise at the right level. If women push themselves too high, they risk placing excessive physical or systemic load on the body or the foetus, but equally if exercise is not intense enough then the positive clinical benefits will not be achieved. So how do we ensure women are exercising at the right level? Let’s look more closely at what the Australian 2016 RANZCOG guidelines say:
Woman are recommended to accumulate 150-300 minutes of moderate intensity physical activity each week, ideally by being active most days for at least 30 mins.
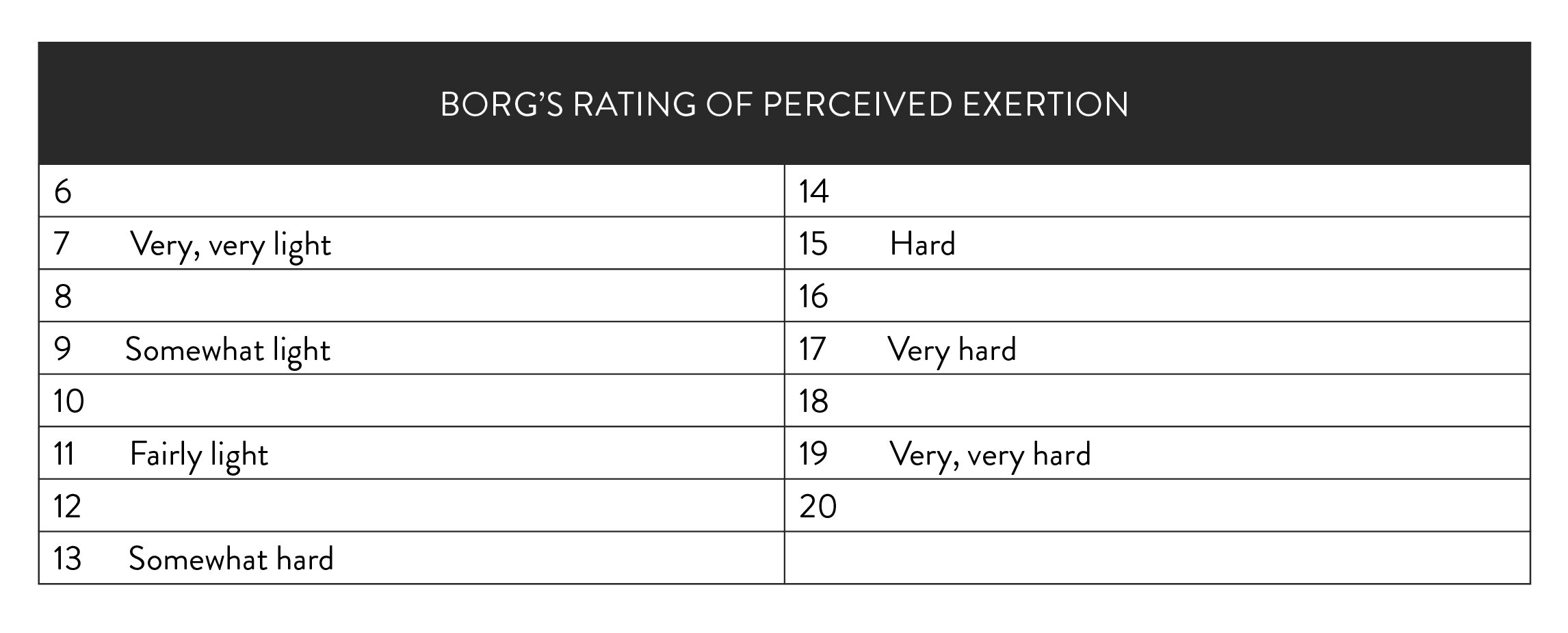
‘Moderate intensity’ will vary from person to person which given that everyone has a different level of fitness and a different response to pregnancy so monitoring this with the Borg scale or the talk test is important and something all pregnant women should be aware of (see below).
Each session should not exceed 60 mins due to reduced ability of the body to thermoregulate (more on that below).
Exercise should be a combination of aerobic style such as brisk walking, running, bike, cross trainer (Note if you are walking it must be brisk).
Exercise should ensure that two days per week strength-based training that includes weights, body weight or resistance bands are used to maintain and improve muscle mass.
The guidelines also state that the pregnant woman should consider her baseline level of fitness and previous exercise, undertake an assessment of her risks prior to commencing. She should also consider the physiological adaptations that occur in pregnancy.
So, we all know that the main physiological adaptation in pregnancy is a belly that grows so large that you can’t even see your own undies, but there are many other adaptations that are occurring below the surface that women ought to aware of that will affect exercise.
The body produces 50% more blood in pregnancy, which means the heart is working a harder to pump this blood around every single second of every single day. This is why when exercising at an intensity that was previously not challenging, in pregnancy it will take your breath away.
There is an increase in the resting heart rate, which means when you exercise the heart rate has less reserve before it starts to hit its higher limits.
There is an anatomical shift of the organs to make space for the placenta and baby, this leads to compression of the diaphragm making it more challenging to breathe.
Hormones continuously released to ensure maintenance of the pregnancy, growth of the baby and in the placenta. This hormonal load especially in the first trimester leads to a very exhausted and nauseated state, which will impact the energy left for exercise.
The veins soften and widen a little resulting in slower return of blood to the heart, and pooling of blood in the extremities and reduced blood pressure. This is one of the reason women get varicose veins in pregnancy. This may lead to a feeling of faintness or light headiness upon standing.
The connective tissue and ligaments make joints, especially the pelvic joints more mobile, and when challenged especially in third trimester may experience pelvic girdle or back pain.
The pelvic floor muscles soften, become spongy and relax in preparation for childbirth, which means they are less supportive of the pelvis and pelvic organs during exercise, making women more prone to leaking or vaginal heaviness.
There is Increase in body weight and change in weight distribution making exercise such as those lying on tummy or with weights directly in front impossible.
There is an increase in the core temperature, and in exercise it is even harder to bring this down. This is important to know as when exposed to heats beyond 39 degrees this may increase the risk of neural tube defects.
Exercise in pregnancy sounds like complicated business, and this is why many people fall into the trap of thinking it’s simply too hard. But it’s really not, and I urge all women to follow these very simply recommendations to ensure they are exercising in a way that is not only safe but is going to create long lasting health benefits for mother and baby.
1. Avoid exercise lying on you back after 17 weeks of pregnancy (The uterus can place excessive pressure on the Vena Cava decreasing blood return to the heart and placenta)
2. Avoid exercising in extremely warm temperatures, hot pools, saunas or spas due to the thermoregulation ability
3. Monitor to ensure you are exercising at a moderate intensity. By doing this you ensure that that baby is getting enough oxygen, and the mother is challenged enough to provide the clinical benefits of exercise.
There are two very simple ways to do this:
The talk test is to means that a woman would be able to can maintain a conversation whilst exercising. So, if you are a well-practiced runner, that can continue to run and could have a conversation then carry on! But if running up a hill and it becomes too hard to talk, then slow down.
The modified borg rating of perceived exertion is a scale that women learn to rate themselves on as exercising at the level of 12 -14 which is Somewhat Hard.
4. Ensure adequate hydration prior to and during exercise as well as nutrition and calorie intake
5. Learn to listen to your body on a daily basis as pregnancy is dynamic and the body is constantly changing. If you aren’t feeling great, you get pain, or are exhausted your body is telling you something. Listen. These days are best as light walk or rest days.
6. If doing weights, keep breathing throughout the load, and do not breath hold (Valsalva) Watch for presence of visible abdominal separation under high loads and seek support from a women’s health Physiotherapist if this occurs.
7. Make pelvic floor exercises as a part of your regime especially if you are doing weights or running due to the impacts that go through the pelvic floor. There is strong evidence that pelvic floor muscle training during pregnancy can prevent and treat urinary incontinence in the postpartum period.
8. Watch for any symptoms such as bleeding, significant shortness of breath, dizziness or other adverse symptoms and seek medical support.
Finally, if you are a woman who is pregnant and have previously been inactive then don’t fear pregnancy is the perfect time to start! The 2019 Canadian Pregnancy Exercise Guidelines state that previously inactive pregnant women not meeting the exercise threshold should be encouraged to do so. This should occur gradually, at a lower intensity and duration and increase as the pregnancy progresses.
Ladies, exercise in pregnancy has without doubt a few considerations, but if you listen to both your body and the guidelines then you can’t go wrong. The benefits of exercise in pregnancy is indisputable, and it really is riskier business flopping on the couch in pregnancy then getting out there for a brisk walk or weight session. So, go on embrace the talk test, listen to your body and get moving mummas!
References:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Exercise during pregnancy 2016 Statement.
Mottola at al. 2019 Canadian guideline for physical activity throughput pregnancy. Br J Sports Med 2018; (52) 1339 - 1346.